NPM1 and FLT3 mutational status assessment is recommended in acute myeloid leukemia (AML) at diagnosis by European Leukemia Net (ELN) risk stratification. The presence of NPM1 mutation (NPM1-mut) partially overcomes the negative prognostic impact of FLT3-ITD, which is also modulated by FLT3-ITD/wild-type allelic ratio. Targeted drugs are available for FLT3-mutated AML but no data are available so far on the efficacy of intensified front-line regimens in overcoming the negative prognostic role of FLT3-ITD mutation.
We investigated the efficacy of an intensive fludarabine, high dose cytarabine (ARA-C) and Idarubicin (IDA) induction regimen (FLAI) as frontline treatment for fit, de novo AML patients according to NPM1 and FLT3-ITD mutational status.
One-hundred and forty-nine consecutive AML patients, treated in 3 Hematology Italian centers from January 2008 to January 2018, were included in this analysis. Twenty nine patients had isolated FLT3-ITD, 59 concomitant FLT3-ITD and NPM1-mut and 61 isolated NPM1-mut. Median age was 51 yrs (range: 18-65). All patients received FLAI induction (fludarabine 30 mg/sqm and ARA-C 2g/sqm on days 1 to 5 plus IDA 10 mg/sqm on days 1-3-5). For patients achieving CR fludarabine was omitted on II induction and IDA dose was increased to 12 mg/sqm. Before ELN 2017 risk stratification was adopted, patients with isolated FLT3-ITD mutation were scheduled to receive allogeneic bone marrow transplantation (allo-BMT) in first CR regardless of allelic burden. For patients with AML with NPM1 mutation and concomitant FLT3-ITD indication to allo-BMT in 1st complete remission was mainly based on minimal residual disease (MRD) status. MRD was evaluated on marrow samples using multicolor flow-cytometry (MFC) or NPM1 expression levels. Negative MFC-MRD was defined by the presence of less than 25 clustered leukemic cells/105 total events (threshold of 0.025%, Minetto et. al, BJH 2019). NPM1-mut (NPM1-A, B and D) was measured using Muta Quant Kit Ipsogen from Qiagen. FLT3-ITD allelic burden was available in31/64 of FLT3-ITD patients.
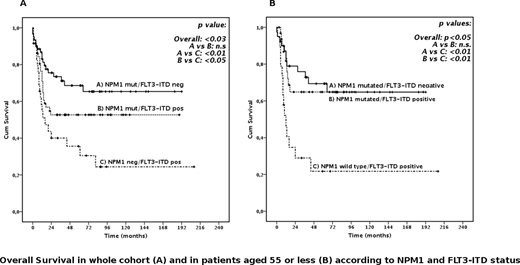
Overall, 60-days mortality was 4.7%. After first induction cycles, 129 patients achieved CR (86.6%). Thirty-five/129 (25.5%) CR patients underwent BMT in first CR. After a median follow up of 68 months, 3-year overall survival (OS) was 58.6% (median not reached). In univariate analysis OS duration was affected by NPM1, FLT3 mutational status and ELN risk score. However, NPM1-mutated patient was not negatively affected by the presence of FLT3-ITD, regardless of allelic burden. This observation was even more evident in patients younger than 55 yrs (3 yy OS 64% and 68% for NPM1-mutated with or w/o FLT3-ITD, respectively (p=n.s, Figure 1), regardless of FLT3-ITD allelic burden. ELN 2017 high risk patients displayed the worst prognosis (3-year OS 35.2%). Multivariate analysis showed that NPM1 mutation was the strongest predictor of survival.
In order to assess the impact of allo-BMT in 1st CR we performed a Landmark Analysis including patients alive and in CR at day 90. Interestingly, performing allo-BMT in 1st CR did not impact OS in the whole cohort of patients and irrespectively of NPM1 and FLT3 mutational status. The only subgroup who benefit from allo-BMT in first CR was high risk ELN2017 (p<0.05).
Despite the potential bias due to the retrospective nature of the analysis, our data indicate that intensive fludarabine-high dose cytarabine-based induction exerts a strong anti-leukemic efficacy in younger AML patients carrying NPM1 mutation irrespectively of FLT3 mutational status. Our data potentially question the role of BMT in first CR in this setting.
Bocchia:CELGENE: Honoraria; Incyte: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal